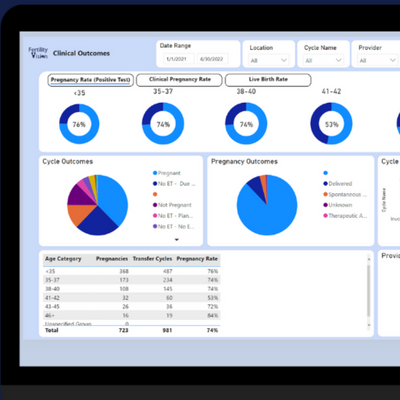
From Harvard to Princeton, our data is used to power important fertility studies including:
To view each study, please click on the topic.
D. Vaughn, L. Murphy, E. Seidler, A. Penzias, D. Sakkas, W. Neuhausser
There have been many medical advances over the years when it comes to embryo culture transfer, and today most fertility clinics choose to employ the blastocyst transfer. But a study done by the Boston IVF set out to look at the implantation rates of early cleavage embryo transfers versus blastocysts transfers. The researchers were concerned that there might be embryos lost in vitro that do not develop between days two and three until day five– while in vivo they might have the opportunity to implant. This is particularly important for women who do not have many embryos available.
This article will discuss:
- The difference between early cleavage embryo transfer and blastocyst transfer
- What the results of the study discover about the viability of implanting embryos in different stages

What is the Difference Between Early Cleavage Embryo Transfer and Blastocyst Transfer?
Embryo transfer refers to the fertility treatment process that transfers the embryo into the uterus of a woman, with the hope of it implanting and developing into a pregnancy. An early embryo transfer refers to placing an embryo that has been cultured for 2-3 days after fertilization into the uterus. If the patient happened to have any embryos in this stage that were not used in implantation, they can be frozen and stored for future use in case the process is not successful.
If there are multiple embryos that develop after fertilization, fertility specialists will see if extra days (typically around day five after fertilization) will allow them to develop into blastocysts. Infertility studies have shown that blastocyst transfer can have a higher success rate for implantation– compared to the early cleavage embryo transfer. This has caused many clinics to focus solely on blastocyst transfer, and lead the researchers behind this study to wonder if this might not be the only option for patients striving for implantation.
Study Objective and Method
This study sought to examine the different outcomes of patients who had less than five 2PN embryos, and who either utilized early cleavage transfer or blastocyst transfer. It also looked at patients who had poor cleavage stage embryos which were transferred at this stage, to those patients who had poor cleavage stage embryos but waited until the blastocyst stage to complete the transfer.
The patients in this study all had oocytes removed from 2013 through 2016, and whose transfers were fresh as opposed to frozen. Cases were included in the cleavage transfer group if the patient had one or more embryos transferred at the cleavage stage on day two or three, as well as those patients who had embryos on day one. Patients were included in the blastocyst transfer group if they had one or more embryos transferred on day four through six.

Results and Conclusions
Patients younger than 38 years old
There 1,183 patients whose data was reviewed for this study, and their results were broken down into two categories– those who were less than 38 years old at transfer, and those that were older than 38 years old at transfer. For those patients who were younger than age 38, there were 668 embryos transferred at the cleavage stage. This resulted in a 21.4% implantation rate and 122 live births. Out of the 409 women who underwent transfers in this group, there was an 18% rate of a live birth via the transfer at the cleavage stage.
For women who were 38 or younger, there were 202 embryos transferred at the blastocyst stage on day five or six. These transfers resulted in a 40.6% implantation rate and amounted to 76 live births. There were 153 transfers done at the blastocyst stage, which amounts to a 38% rate of a live birth.
Patients older than 38 years old
Of the 538 women who were 38 years and older who had 1312 embryos transferred via a cleavage transfer, there was a 7.5% rate of implantation and 61 live births. Out of this subset, this accounts for just 5% of women who gave birth in this group. The 83 women who were 38 years and older and had 155 embryos transferred via a blastocyst transfer had an implantation rate of 19% and 22 live births.
These results show that there is a higher rate of attrition among poor quality in vitro between day three and day five than there is in vivo. The researchers also noted that the birth rate among the transfers at the cleavage stage was poor, however the total live birth rate among blastocyst embryos of 28.6% was encouraging.
The data shows that there are differences between the success rates of the two embryonic transfer techniques, and while these can be dependent upon many factors– including age– the researchers suggest more in depth trials to investigate further.
Publication
Non-inferiority of Cleavage-Stage Versus Blastocyst-Stage Embryo Transfer in Poor Prognosis IVF Patients (PRECiSE Trial): Study Protocol for a Randomized Controlled Trial
Reproductive Health– 17, Article number: 16 (2020)
E. Neuber, M.S. Yohe, A. Bartolucci
On October 1, 2005, the Connecticut Senate Bill No. 508 passed through the CT Senate and the House of Representatives, which required insurance carriers to cover IVF treatment costs. Since 2017, 15 states have introduced legislation that would mandate the coverage of fertility treatments. This mandate would cover assisted reproductive technology (ART) such as IVF treatments, and provide insurance covered assistance to women seeking fertility treatment. The CT law came with a stipulation however, that the coverage is limited until the date of the woman’s 40th birthday. Thankfully for couples seeking fertility treatment in CT, this stipulation was repealed in 2016 and now insurance companies are required to remove all age limits, as studies have repeatedly shown that IVF treatment is effective in women over 40 years of age.
Infertility treatments have helped many couples become parents, but the procedures can be quite costly. IVF cycles can range anywhere from $12,000-$17,000, which leads some states to wonder if insurance plans should cover them. The chance of conception and pregnancy via IVF depends on many factors, including the age of the woman and whether or not her eggs are used in the process. It is also important to note that IVF pregnancies can also be at a higher risk of complications as well.
This study examined how lifting this age barrier has impacted women seeking infertility treatment in CT who are over the age of 40. In this article we will:
- Learn the what benefits came from lifting the age limit
- See how access to fertility care in CT has affected women
Hypothesis
The researchers set out with a hypothesis that once the age restrictions of the CT mandate were removed, there would be more women over the age of 40 who would take advantage of the insurance-covered IVF treatment. They also conjectured that in the future, more and more women over the age of 40 would take advantage of this treatment. As more women are made aware through their providers that IVF treatment is covered for their age group, they may consider participating in the treatment themselves.

Results and Discussion
Relying on the information in the eIVF databases, the researchers were able to discern that from 2015-2017 the amount of total IVF procedures increased nationally from 43,447 cycles to 62,610 cycles. They also found out that not only did the total amount of IVF cycles increase, it also increased for women 40 years and over. The percentage of over 40 IVF cycles in 2015 was 26.3%, and increased to 26.4% in 2016. In 2017 the percentage of over 40 women requesting IVF treatment had increased to 28.3%. This could be attributed to not only an increase in overall procedures, but also due to the age mandate being lifted from the procedure as well.
The same trend was seen when observing cycles to retrieval in Connecticut. From 2015-2018, researchers viewed a significant increase in the amount of women age 40 and over with cycles to retrieval, beginning in 2016 when the age mandate was lifted. In 2015, 12.6% of cycles to retrieval were for women age 40 and over, while in 2017, women over 40 accounted for 25.7% of cycles to retrieval. The increase in both the number of IVF cycles and the cycles to retrieval show that not only are more women interested in receiving IVF treatment, but more women age 40 and over are as well.
What does this mean for potential IVF patients?
The median age of the residents of many of Connecticut’s municipalities rose over the past ten years, and now rests at 40.8 years. As the results of this study show, women over the age of 40 are in most need of access to IVF treatment, and they are interested in receiving it. Although the likelihood of pregnancy after 40 is lower than at other ages, there is still a viable chance for IVF to be successful. At the end of 2015, CT enacted on a large scale campaign to notify and inform women of the age mandate change, and it has proven to be very successful if the results of the data are any indication.
Women over 40 are capable of successfully completing IVF treatment, and women should not be barred from this procedure due to their age. The results of this study should be encouraging to all women who are seeking out IVF treatment, especially those that are older. It is also shows that by eliminating a restrictive age mandate, a state can offer their residents access to insurance covered care that they are in need of.
L. Ghidei, C. Raker, L. Brayboy
Racial Disparity in Healthcare
Racial disparity in the U.S. healthcare system is prevalent problem that affects the lives of many minorities as well as the outcomes of various procedures, including IVF. Black and hispanic populations are more likely to receive poorer healthcare from their providers than are white people, which can lead to an increased amount of negative health conditions and death. Studies have shown thatblack populationsare more likely to receive older and more conservative treatments than white people, which can have a profound effect on their lives. It appears this is not just a poverty issue either, as minorities continue to be affected by biases regardless of insurance status, age, and income.
This is partly due to implicit bias held by physicians in all specializations, including those fertility clinics. A recent study funded by a New England Fertility Society grant looked at what is causing black women to experience such disparate outcomes in their IVF treatment.
In this article, we’re going to examine:
- What is causing black women’s varying degrees of success with IVF?
- What can be done to create better chances of IVF success?
Methods of the Study
How researchers examined this issue
There are many reasons that women choose to undergo IVF treatment, but regardless of why, all of them are focused on the same result– to become pregnant and deliver successfully. The success of an IVF cycle depends on a variety of factors, including the age of the woman, and whether or not she is able to use her own eggs or not. If a woman in her mid-30s chooses to undergo IVF and is using her own eggs, there is a greater chance of pregnancy than if a 40 year old woman underwent the same procedure but was using donated eggs. As women age, the chance for a miscarriage also increases, further lowering the chances of a viable pregnancy.
But what if age and egg viability were not the only main factors influencing the success of an IVF treatment? This study looked at the factors that determine the IVF outcomes of black women. In order to do so, researchers utilized the data from eIVF database and subjects were chosen if they at least had one embryo transferred during IVF. The outcomes that were examined were: spontaneous abortion rate, clinical pregnancy rate, and live birth rate.

Results and Conclusions
Black women are less successful with IVF
Out of the 175,796 patients examined, 2.6% patients were Black, 26% were White, and 3% were Hispanic/Latina. The study found that Black women in this data group were more likely to be over 35 when starting their IVF treatment– 61% Black to 50% White. Knowing that age is a major factor in IVF success, this is an interesting observation. Black women in the study were also significantly more likely to be obese when beginning treatment. Thirty six percent of the Black women were considered obese according to their BMI, compared to 22% of White women. Diet and exercise are extremely important to pregnancy overall, and obesity can decrease a woman’s chances of a successful pregnancy.
Another area where researchers saw a disparity with the Black women in the study was with their rates of a tubal or uterine factor. Black women had over 50% greater chance of a tubal factor with 19.8% experiencing this issue compared to 8.6% of White women experiencing the same. Black women also experienced a greater rate of uterine factor compared to White women, with a 7.4% chance compared to 3.1%.
An interesting finding in this study was that Black women were more likely than White women to be under more psychological stress. Just like maintaining a healthy weight, reducing stress is an important component to pregnancy.
When compared to all races examined, Black women had the lowest percentage of clinical pregnancies with 46% of women in the data group. White women had a 55% clinical pregnancy rate, Hispanic/Latina had 60%, and Asian was at 62%. Coupled with the fact that the live birth rate for Black women was 45% less than White women and 30% less than Hispanic/Latina women, and we can further see that there is a significant disparity here. The lower percentage of live birth rate for Black women continued even when the patient characteristics (BMI, infertility diagnosis, diabetes, etc.) were changed.
Conclusions
This data lead the researchers to conclude that Black women can expect less chance of a successful IVF treatment. This is not only the result of disparity and bias in the healthcare system, but it is also due to their older age starting IVF, higher BMI, greater chance of tubal or uterine factors, stress, hypertension, and diabetes.
In order to increase the chances of a successful IVF treatment, it is important to maintain a healthy weight and look for ways to reduce stress. This lifestyle changes can reduce the risk of diabetes and hypertension and may increase the chances of pregnancy.
Publication
Factors associated with disparate outcomes among African American women undergoing IVF
Fertility and Sterility, September 2018,Volume 110, Issue 4, Supplement, Pages e276–e277
T. Xu, S. Malhalingaiah, I. Paschalidis
In a study done with Boston University School of Medicine, the National Science Foundation, and the Center for Information Systems and Engineering, researchers aimed to create a method that would assist in the prediction of the success rate of a patient’s first IVF cycle. This study looked at patients who were doing their first IVF cycle and using their own eggs, and the method was tested against their outcomes.
In this article we’re going to examine:
- How researchers arrived at their prediction model
- How accurate at predicting IVF outcomes is their statistical model
IVF and Eggs
When patients are interested in starting an IVF cycle, they will first need to determine if they are capable of using their own eggs– or if donor eggs are required. Most women prefer to use their own eggs if possible, but sometimes factors such as age or health issues can affect this decision. Many women who are over the age of 40, and who want to use their own eggs, are at times discouraged from doing so. This is due to the fact that as a woman ages, her eggs also age as well. There is less likelihood that the IVF will be successful using the eggs of an over-40 woman.
This is not to say that it cannot be done, it just less likely. IVF is a costly procedure and most patients want to have the best chance possible at a pregnancy, so if they are recommended to do so, will accept the use of donor eggs. However, fertility clinics are available to treat over-40 women with a diminished ovarian reserve (DOR), and who want to use their own eggs. This is possible through customized IVF treatment plans and techniques such as early egg retrieval. This occurs when immature eggs are removed and allowed to mature in the lab via in vitro maturation (IVM). This increases the number of embryos available for implantation and can increase the chance of a pregnancy.

Study Design and Methods
This study examined 22,763 patients using the data from the eIVF database, and sought to find a way to predict the outcomes of these IVF patients during their first cycle of fertility treatment. The prediction accuracy metrics used were AUC and AUC-PR. First, diagnoses were grouped into seven classifications, and a one-hot coding was used for all possible features. The data was randomly divided into test and training sets and feature standardization was used. The performance criteria was measured with AUC=0.5 with random guessing and AUC-PR=percentage of positive samples with random guessing.
Results and Conclusion
For each patient, a series of medical factors were considered such as age, race, lifestyle, and body mass index (BMI). In addition, there were conditions relating to the egg and sperm taken into account as well. For each egg this included the total embryos cryoed, transfer count, and if the embryos were frozen after day five. For the sperm, the volume, concentration, motility, and progression were taken into consideration. In addition, hormone values were accounted for, and the data from day three ovarian test values were taken for: estradiol, progesterone, luteinizing hormone, follicle stimulating hormone, endometrium thickness, antral follicle count, as well as the maximum amount of estradiol.
The results were broken into four categories, age, race, diagnosis, BMI, and the outcome of pregnant and not pregnant was examined against these factors. For women less than 35, 55% of the sample were estimated to be pregnant and 40% were not. For women ages 38-40, only 16% had an outcome of pregnancy, while 21% did not. The chance of pregnancy drops off sharply after 40 years of age according to the analysis, with only 2% of women predicted to be pregnant and 7% were not.

When the results are broken down according to race, the researchers found that White women were the most likely to become pregnant at 22%, but this is also due to the fact that this race category contained the most patients. Asian women were predicted to have the outcome of pregnant after the first cycle of IVF at 4%, Hispanic/Latina at 2%, and Black women at 1%.
The reason for infertility was also examined, and when female infertility was the diagnosis, 45% of patients were estimated to be pregnant, and 14% were not. When there was a male infertility problem, 11% of the patients ended up pregnant while 6% did not have the outcome of pregnancy. If the diagnosis was tubal problems, it was an almost even percentage, with 5% pregnant and 4% not pregnant.
Finally, when the results are broken down according to BMI, the patients who had a BMI of 18.5-24.9 were the most likely to be pregnant, with 42% of women. As BMIs increase, the percentage of women who became pregnant drops. Those with BMIs lower than 18.5, only 2% would end up with a pregnant outcome.
The model used for this analysis achieved an accuracy of 69.11% in AUC and 67.57% in AUC-PR, which means this model is useful to help predict the success rate of an IVF treatment. As this study shows, the success rate of the first cycle of IVF is dependent on many things, each of which can play a part in a pregnancy result.
- Should Fertility Clinics Utilize Both Early Cleavage Embryo Transfers and Blastocyst Transfers?
-
D. Vaughn, L. Murphy, E. Seidler, A. Penzias, D. Sakkas, W. Neuhausser
There have been many medical advances over the years when it comes to embryo culture transfer, and today most fertility clinics choose to employ the blastocyst transfer. But a study done by the Boston IVF set out to look at the implantation rates of early cleavage embryo transfers versus blastocysts transfers. The researchers were concerned that there might be embryos lost in vitro that do not develop between days two and three until day five– while in vivo they might have the opportunity to implant. This is particularly important for women who do not have many embryos available.
This article will discuss:
- The difference between early cleavage embryo transfer and blastocyst transfer
- What the results of the study discover about the viability of implanting embryos in different stages

What is the Difference Between Early Cleavage Embryo Transfer and Blastocyst Transfer?
Embryo transfer refers to the fertility treatment process that transfers the embryo into the uterus of a woman, with the hope of it implanting and developing into a pregnancy. An early embryo transfer refers to placing an embryo that has been cultured for 2-3 days after fertilization into the uterus. If the patient happened to have any embryos in this stage that were not used in implantation, they can be frozen and stored for future use in case the process is not successful.
If there are multiple embryos that develop after fertilization, fertility specialists will see if extra days (typically around day five after fertilization) will allow them to develop into blastocysts. Infertility studies have shown that blastocyst transfer can have a higher success rate for implantation– compared to the early cleavage embryo transfer. This has caused many clinics to focus solely on blastocyst transfer, and lead the researchers behind this study to wonder if this might not be the only option for patients striving for implantation.
Study Objective and Method
This study sought to examine the different outcomes of patients who had less than five 2PN embryos, and who either utilized early cleavage transfer or blastocyst transfer. It also looked at patients who had poor cleavage stage embryos which were transferred at this stage, to those patients who had poor cleavage stage embryos but waited until the blastocyst stage to complete the transfer.
The patients in this study all had oocytes removed from 2013 through 2016, and whose transfers were fresh as opposed to frozen. Cases were included in the cleavage transfer group if the patient had one or more embryos transferred at the cleavage stage on day two or three, as well as those patients who had embryos on day one. Patients were included in the blastocyst transfer group if they had one or more embryos transferred on day four through six.

Measuring the birth rate of both embryonic transfers may assist in deciding which offers the most benefit to individuals. Image courtesy of the Cleveland Clinic. Results and Conclusions
Patients younger than 38 years old
There 1,183 patients whose data was reviewed for this study, and their results were broken down into two categories– those who were less than 38 years old at transfer, and those that were older than 38 years old at transfer. For those patients who were younger than age 38, there were 668 embryos transferred at the cleavage stage. This resulted in a 21.4% implantation rate and 122 live births. Out of the 409 women who underwent transfers in this group, there was an 18% rate of a live birth via the transfer at the cleavage stage.
For women who were 38 or younger, there were 202 embryos transferred at the blastocyst stage on day five or six. These transfers resulted in a 40.6% implantation rate and amounted to 76 live births. There were 153 transfers done at the blastocyst stage, which amounts to a 38% rate of a live birth.
Patients older than 38 years old
Of the 538 women who were 38 years and older who had 1312 embryos transferred via a cleavage transfer, there was a 7.5% rate of implantation and 61 live births. Out of this subset, this accounts for just 5% of women who gave birth in this group. The 83 women who were 38 years and older and had 155 embryos transferred via a blastocyst transfer had an implantation rate of 19% and 22 live births.
These results show that there is a higher rate of attrition among poor quality in vitro between day three and day five than there is in vivo. The researchers also noted that the birth rate among the transfers at the cleavage stage was poor, however the total live birth rate among blastocyst embryos of 28.6% was encouraging.
The data shows that there are differences between the success rates of the two embryonic transfer techniques, and while these can be dependent upon many factors– including age– the researchers suggest more in depth trials to investigate further.
Publication
Non-inferiority of Cleavage-Stage Versus Blastocyst-Stage Embryo Transfer in Poor Prognosis IVF Patients (PRECiSE Trial): Study Protocol for a Randomized Controlled Trial
Reproductive Health– 17, Article number: 16 (2020)
- How Did Removing the Age Limit to IVF Treatment Affect Access to Care in Connecticut?
-
E. Neuber, M.S. Yohe, A. Bartolucci
On October 1, 2005, the Connecticut Senate Bill No. 508 passed through the CT Senate and the House of Representatives, which required insurance carriers to cover IVF treatment costs. Since 2017, 15 states have introduced legislation that would mandate the coverage of fertility treatments. This mandate would cover assisted reproductive technology (ART) such as IVF treatments, and provide insurance covered assistance to women seeking fertility treatment. The CT law came with a stipulation however, that the coverage is limited until the date of the woman’s 40th birthday. Thankfully for couples seeking fertility treatment in CT, this stipulation was repealed in 2016 and now insurance companies are required to remove all age limits, as studies have repeatedly shown that IVF treatment is effective in women over 40 years of age.
Infertility treatments have helped many couples become parents, but the procedures can be quite costly. IVF cycles can range anywhere from $12,000-$17,000, which leads some states to wonder if insurance plans should cover them. The chance of conception and pregnancy via IVF depends on many factors, including the age of the woman and whether or not her eggs are used in the process. It is also important to note that IVF pregnancies can also be at a higher risk of complications as well.
This study examined how lifting this age barrier has impacted women seeking infertility treatment in CT who are over the age of 40. In this article we will:
- Learn the what benefits came from lifting the age limit
- See how access to fertility care in CT has affected women
Hypothesis
The researchers set out with a hypothesis that once the age restrictions of the CT mandate were removed, there would be more women over the age of 40 who would take advantage of the insurance-covered IVF treatment. They also conjectured that in the future, more and more women over the age of 40 would take advantage of this treatment. As more women are made aware through their providers that IVF treatment is covered for their age group, they may consider participating in the treatment themselves.

Results and Discussion
Relying on the information in the eIVF databases, the researchers were able to discern that from 2015-2017 the amount of total IVF procedures increased nationally from 43,447 cycles to 62,610 cycles. They also found out that not only did the total amount of IVF cycles increase, it also increased for women 40 years and over. The percentage of over 40 IVF cycles in 2015 was 26.3%, and increased to 26.4% in 2016. In 2017 the percentage of over 40 women requesting IVF treatment had increased to 28.3%. This could be attributed to not only an increase in overall procedures, but also due to the age mandate being lifted from the procedure as well.
The same trend was seen when observing cycles to retrieval in Connecticut. From 2015-2018, researchers viewed a significant increase in the amount of women age 40 and over with cycles to retrieval, beginning in 2016 when the age mandate was lifted. In 2015, 12.6% of cycles to retrieval were for women age 40 and over, while in 2017, women over 40 accounted for 25.7% of cycles to retrieval. The increase in both the number of IVF cycles and the cycles to retrieval show that not only are more women interested in receiving IVF treatment, but more women age 40 and over are as well.
What does this mean for potential IVF patients?
The median age of the residents of many of Connecticut’s municipalities rose over the past ten years, and now rests at 40.8 years. As the results of this study show, women over the age of 40 are in most need of access to IVF treatment, and they are interested in receiving it. Although the likelihood of pregnancy after 40 is lower than at other ages, there is still a viable chance for IVF to be successful. At the end of 2015, CT enacted on a large scale campaign to notify and inform women of the age mandate change, and it has proven to be very successful if the results of the data are any indication.
Women over 40 are capable of successfully completing IVF treatment, and women should not be barred from this procedure due to their age. The results of this study should be encouraging to all women who are seeking out IVF treatment, especially those that are older. It is also shows that by eliminating a restrictive age mandate, a state can offer their residents access to insurance covered care that they are in need of.
- Disparate Outcomes with IVF Among Black Women
-
L. Ghidei, C. Raker, L. Brayboy
Racial Disparity in Healthcare
Racial disparity in the U.S. healthcare system is prevalent problem that affects the lives of many minorities as well as the outcomes of various procedures, including IVF. Black and hispanic populations are more likely to receive poorer healthcare from their providers than are white people, which can lead to an increased amount of negative health conditions and death. Studies have shown thatblack populationsare more likely to receive older and more conservative treatments than white people, which can have a profound effect on their lives. It appears this is not just a poverty issue either, as minorities continue to be affected by biases regardless of insurance status, age, and income.
This is partly due to implicit bias held by physicians in all specializations, including those fertility clinics. A recent study funded by a New England Fertility Society grant looked at what is causing black women to experience such disparate outcomes in their IVF treatment.
In this article, we’re going to examine:
- What is causing black women’s varying degrees of success with IVF?
- What can be done to create better chances of IVF success?
Methods of the Study
How researchers examined this issue
There are many reasons that women choose to undergo IVF treatment, but regardless of why, all of them are focused on the same result– to become pregnant and deliver successfully. The success of an IVF cycle depends on a variety of factors, including the age of the woman, and whether or not she is able to use her own eggs or not. If a woman in her mid-30s chooses to undergo IVF and is using her own eggs, there is a greater chance of pregnancy than if a 40 year old woman underwent the same procedure but was using donated eggs. As women age, the chance for a miscarriage also increases, further lowering the chances of a viable pregnancy.
But what if age and egg viability were not the only main factors influencing the success of an IVF treatment? This study looked at the factors that determine the IVF outcomes of black women. In order to do so, researchers utilized the data from eIVF database and subjects were chosen if they at least had one embryo transferred during IVF. The outcomes that were examined were: spontaneous abortion rate, clinical pregnancy rate, and live birth rate.

Black women were less likely to find success with IVF treatment for a variety of reasons. Results and Conclusions
Black women are less successful with IVF
Out of the 175,796 patients examined, 2.6% patients were Black, 26% were White, and 3% were Hispanic/Latina. The study found that Black women in this data group were more likely to be over 35 when starting their IVF treatment– 61% Black to 50% White. Knowing that age is a major factor in IVF success, this is an interesting observation. Black women in the study were also significantly more likely to be obese when beginning treatment. Thirty six percent of the Black women were considered obese according to their BMI, compared to 22% of White women. Diet and exercise are extremely important to pregnancy overall, and obesity can decrease a woman’s chances of a successful pregnancy.
Another area where researchers saw a disparity with the Black women in the study was with their rates of a tubal or uterine factor. Black women had over 50% greater chance of a tubal factor with 19.8% experiencing this issue compared to 8.6% of White women experiencing the same. Black women also experienced a greater rate of uterine factor compared to White women, with a 7.4% chance compared to 3.1%.
An interesting finding in this study was that Black women were more likely than White women to be under more psychological stress. Just like maintaining a healthy weight, reducing stress is an important component to pregnancy.
When compared to all races examined, Black women had the lowest percentage of clinical pregnancies with 46% of women in the data group. White women had a 55% clinical pregnancy rate, Hispanic/Latina had 60%, and Asian was at 62%. Coupled with the fact that the live birth rate for Black women was 45% less than White women and 30% less than Hispanic/Latina women, and we can further see that there is a significant disparity here. The lower percentage of live birth rate for Black women continued even when the patient characteristics (BMI, infertility diagnosis, diabetes, etc.) were changed.
Conclusions
This data lead the researchers to conclude that Black women can expect less chance of a successful IVF treatment. This is not only the result of disparity and bias in the healthcare system, but it is also due to their older age starting IVF, higher BMI, greater chance of tubal or uterine factors, stress, hypertension, and diabetes.
In order to increase the chances of a successful IVF treatment, it is important to maintain a healthy weight and look for ways to reduce stress. This lifestyle changes can reduce the risk of diabetes and hypertension and may increase the chances of pregnancy.
Publication
Factors associated with disparate outcomes among African American women undergoing IVF
Fertility and Sterility, September 2018,Volume 110, Issue 4, Supplement, Pages e276–e277 - In-Cycle Outcome Prediction Classification for IVF Treatment
-
T. Xu, S. Malhalingaiah, I. Paschalidis
In a study done with Boston University School of Medicine, the National Science Foundation, and the Center for Information Systems and Engineering, researchers aimed to create a method that would assist in the prediction of the success rate of a patient’s first IVF cycle. This study looked at patients who were doing their first IVF cycle and using their own eggs, and the method was tested against their outcomes.
In this article we’re going to examine:
- How researchers arrived at their prediction model
- How accurate at predicting IVF outcomes is their statistical model
IVF and Eggs
When patients are interested in starting an IVF cycle, they will first need to determine if they are capable of using their own eggs– or if donor eggs are required. Most women prefer to use their own eggs if possible, but sometimes factors such as age or health issues can affect this decision. Many women who are over the age of 40, and who want to use their own eggs, are at times discouraged from doing so. This is due to the fact that as a woman ages, her eggs also age as well. There is less likelihood that the IVF will be successful using the eggs of an over-40 woman.
This is not to say that it cannot be done, it just less likely. IVF is a costly procedure and most patients want to have the best chance possible at a pregnancy, so if they are recommended to do so, will accept the use of donor eggs. However, fertility clinics are available to treat over-40 women with a diminished ovarian reserve (DOR), and who want to use their own eggs. This is possible through customized IVF treatment plans and techniques such as early egg retrieval. This occurs when immature eggs are removed and allowed to mature in the lab via in vitro maturation (IVM). This increases the number of embryos available for implantation and can increase the chance of a pregnancy.

As this study shows, there are many factors at play when it comes to a successful IVF cycle. Study Design and Methods
This study examined 22,763 patients using the data from the eIVF database, and sought to find a way to predict the outcomes of these IVF patients during their first cycle of fertility treatment. The prediction accuracy metrics used were AUC and AUC-PR. First, diagnoses were grouped into seven classifications, and a one-hot coding was used for all possible features. The data was randomly divided into test and training sets and feature standardization was used. The performance criteria was measured with AUC=0.5 with random guessing and AUC-PR=percentage of positive samples with random guessing.
Results and Conclusion
For each patient, a series of medical factors were considered such as age, race, lifestyle, and body mass index (BMI). In addition, there were conditions relating to the egg and sperm taken into account as well. For each egg this included the total embryos cryoed, transfer count, and if the embryos were frozen after day five. For the sperm, the volume, concentration, motility, and progression were taken into consideration. In addition, hormone values were accounted for, and the data from day three ovarian test values were taken for: estradiol, progesterone, luteinizing hormone, follicle stimulating hormone, endometrium thickness, antral follicle count, as well as the maximum amount of estradiol.
The results were broken into four categories, age, race, diagnosis, BMI, and the outcome of pregnant and not pregnant was examined against these factors. For women less than 35, 55% of the sample were estimated to be pregnant and 40% were not. For women ages 38-40, only 16% had an outcome of pregnancy, while 21% did not. The chance of pregnancy drops off sharply after 40 years of age according to the analysis, with only 2% of women predicted to be pregnant and 7% were not.

The study’s predictive results were broken down into four demographic categories. Table courtesy ofBoston University School of Medicine.
When the results are broken down according to race, the researchers found that White women were the most likely to become pregnant at 22%, but this is also due to the fact that this race category contained the most patients. Asian women were predicted to have the outcome of pregnant after the first cycle of IVF at 4%, Hispanic/Latina at 2%, and Black women at 1%.
The reason for infertility was also examined, and when female infertility was the diagnosis, 45% of patients were estimated to be pregnant, and 14% were not. When there was a male infertility problem, 11% of the patients ended up pregnant while 6% did not have the outcome of pregnancy. If the diagnosis was tubal problems, it was an almost even percentage, with 5% pregnant and 4% not pregnant.
Finally, when the results are broken down according to BMI, the patients who had a BMI of 18.5-24.9 were the most likely to be pregnant, with 42% of women. As BMIs increase, the percentage of women who became pregnant drops. Those with BMIs lower than 18.5, only 2% would end up with a pregnant outcome.
The model used for this analysis achieved an accuracy of 69.11% in AUC and 67.57% in AUC-PR, which means this model is useful to help predict the success rate of an IVF treatment. As this study shows, the success rate of the first cycle of IVF is dependent on many things, each of which can play a part in a pregnancy result.